New MSI-H Cancer Treatment
New MSI-H Cancer Treatment
introduction
An eLife study shows that WRN (Werner syndrome helicase) holds promise for the treatment of patients with high-grade microsatellite instability (MSI) tumors. Microsatellite instability (MSI) refers to the loss of mismatch repair (MMR) gene function, resulting in the loss of erroneous insertions and deletions of DNA. Growth or truncation of MSI tumor microsatellite sequences compared to normal tissue is one of the hallmarks of DNA repair-deficient tumor cells.
Microsatellite Instability
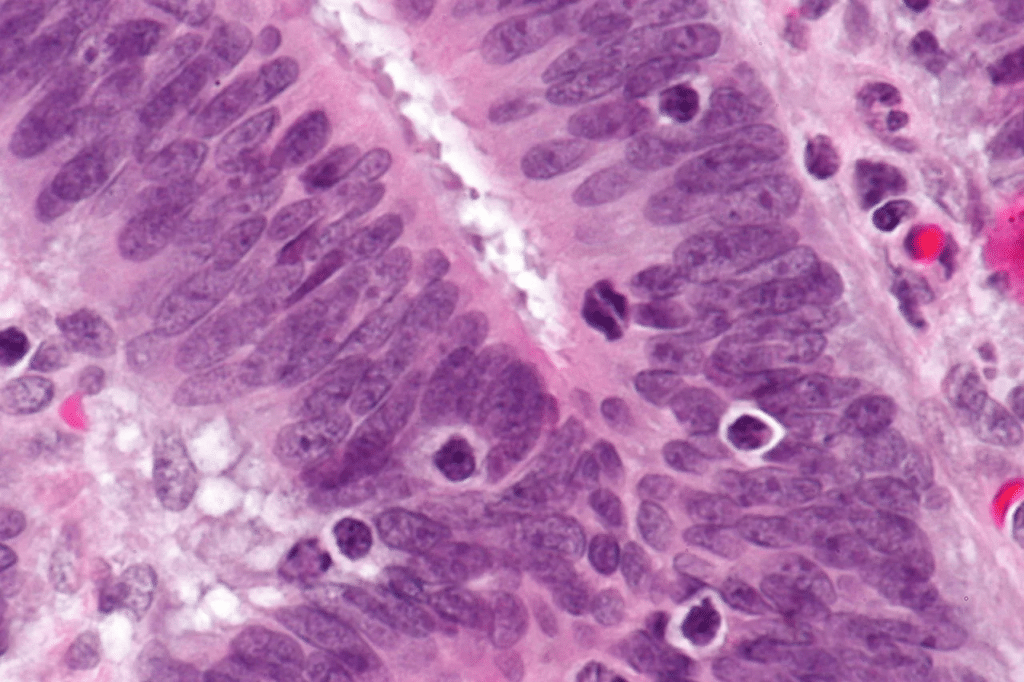
Microsatellite instability (MSI) is the condition of genetic hypermutability (predisposition to mutation) that results from impaired DNA mismatch repair (MMR). The presence of MSI represents phenotypic evidence that MMR is not functioning normally. MSI was discovered in the 1970s and 1980s. In a broad sense, MSI results from the inability of the mismatch repair (MMR) proteins to fix a DNA replication error. DNA replication occurs in the “S” phase of the cell cycle; the faulty event creating an MSI region occurs during the second replication event. The original strand is unharmed, but the daughter strand experiences a frame-shift mutation due to DNA polymerase slippage. Specifically, DNA polymerase slips, creating a temporary insertion-deletion loop, which is usually recognized by MMR proteins. However, when the MMR proteins do not function normally, as in the case of MSI, this loop results in frame-shift mutations, either through insertions or deletions, yielding non-functioning proteins.
In May 2017, the FDA approved the PD-L1 immunosuppressant Pabloizumab for the treatment of unresectable or metastatic solid tumors with MSI-H or mismatch repair deficiency (dMMR). Immunotherapies such as pembrolizumab, nivolumab, and ipilimumab have transformed the treatment of MSI-H tumors. Although these drugs often cause long-term positive responses in MSI-H cancer patients, eventual resistance to immunotherapy means more effective treatments are still needed. According to Simon Wöhrle, chief scientist at the Boehringer Ingelheim Regional Center (RCV) in Vienna, Austria, targeted cancer therapy should be based on biological systems that rely on tumor cells rather than healthy tissue for survival. Therefore, before developing new treatments for MSI-H cancer cells, we first need to understand what helps them survive and grow.
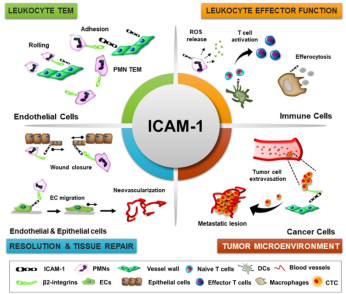
The team used MSI-H cancer cell analysis and recent cell line functional screening data to find out. They showed that removing WRN from MSI-H cells prevents them from working properly and leads to defective cell division. Importantly, they found that WRN-deficient MSI-H cell lines showed chromosome disruption and genomic instability, suggesting that WRN is a novel vulnerability of MSI-H cells. Previous studies have shown that WRN loss leads to Werner syndrome, in which premature aging is associated with an increased lifetime risk of tumor development. Researchers have demonstrated the ability to combine deep functional genomic screening data with tumor cell line analysis to identify novel targets in oncology. The results of this study suggest that pharmacological inhibition of WRN function may be a new targeted therapy strategy for MSI-H cancer, helping to meet the need for more effective drugs.